Making Medicare’s 8 Minute Rule When billing for rehabilitation services provided to Medicare beneficiaries, the Centers for Medicare and Medicaid Services (CMS) requires therapists adhere to what’s referred to as the “8 Minute Rule”. This term is a little misleading as it seems to imply if you do at least …

When billing for rehabilitation services provided to Medicare beneficiaries, the Centers for Medicare and Medicaid Services (CMS) requires therapists adhere to what’s referred to as the “8 Minute Rule”. This term is a little misleading as it seems to imply if you do at least 8 minutes of any procedure defined as a timed code you may bill 1 unit for that. Unfortunately, as is often true with CMS, it’s not that simple.
Let’s first start with reviewing timed codes and how you “time” your services. According to the Local Coverage Determination (LCD) from the Medicare Administrative Contractor National Government Services (found here), timed codes are those defined as requiring one-on-one care. This means you are only attending to that patient during the time the service is being provided, and that time is spent providing skilled services. In other words, you cannot be working with another patient or doing documentation or anything else at the same time.
It also means that you must be the one providing the procedure. Any service provided by an aide is considered unskilled, therefore unbillable, and does not meet the one-on-one definition. Further, time spent resting, changing, waiting for equipment, for example, is not skilled care, and thus not billable time. Conversely, time spent determining the patient’s status that day, how they tolerated the previous session, or whether there was a change in their medical status would be considered “skilled”, and therefore billable time.
Un-timed codes also referred to as service-based CPT codes do not have a time requirement in their definition and are typically provided to a patient only once per day. These codes would include Physical Therapy Evaluation (97161), Mechanical Traction (97012) or Electrical Stim, unattended (97014). Only one unit of these codes are billed regardless of how long they are done to the patient. Since there is no timed component these codes are billed as 1 unit but are not included in the totaling of the timed code units.
Time based codes are defined in the AMA CPT code book as those services being administered one-on-one in 15-minute blocks of time, e.g. 1 unit = 15 minutes. This is where the 8-minute rule comes into play in determining the number of units that can be billed for that visit.
The simplest way to consider this is to add up all the time spent providing these timed codes. For each 15 minutes of one service you would bill 1 unit of that code. If there is at least an additional 8 minutes left over, you may bill another unit. If you have 7 minutes left over you cannot bill for that. For example, if you provided a total of 38 minutes of one-on-one care of timed codes then you may bill 3 units. But if you do 37 minutes of care you can only bill for 2 units.
With all the above in mind let’s consider how the 8 minute rule is applied correctly. First, you should total all the time spent on timed procedures and modalities (like ultrasound or attended e-stim). This should exclude any time spent on untimed codes like many modalities or evaluations/re-evaluations. Utilizing the chart below (from www.ngsmedicare.com) you should determine the total number of timed coding units you may bill.
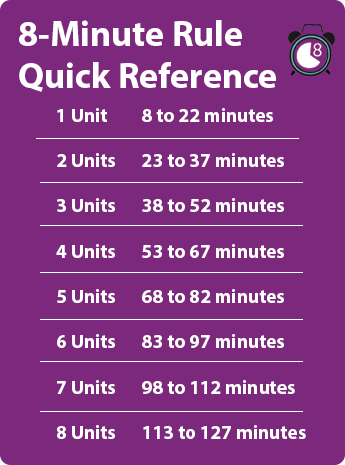
If the total time of timed procedures is 28 minutes you may bill 2 units of timed codes (eg: 15+7) or if you’ve done 56 minutes of timed procedures you may bill 4 units of codes, and so on.
Next you will need to determine which codes to appropriately assign the correct number of units. This has to be done based on the number of minutes each service was provided although there are some caveats. First for any service provided for at least 15 minutes you must bill 1 unit. Sometimes that’s easy: if you provide 15 minutes of Therapeutic Exercise you bill 1 unit of that code, 30 minutes of Neuromuscular Re-education is 2 units of that code.
But let’s look at some examples of how you bill when you have total time not evenly allotted to 15 minute increments, which is most typical:
Let’s say you do:
25 minutes of therapeutic exercises + 23 minutes of therapeutic activities = 48 minutes total
Using the chart above you see you will bill 3 units. You must bill 1 unit of therapeutic exercise and 1 unit of therapeutic activities. But you have 10 min of therapeutic exercise left over and 8 minutes of therapeutic activities remaining. You now need to bill the code for which you have the most remainder minutes (therapeutic exercises). So you add the therapeutic activities minutes to the therapeutic exercise minutes and bill one more unit of therapeutic exercises.
Here’s another one:
32 minutes of therapeutic exercises + 7 minutes of manual therapy = 39 minutes
According to the chart you can bill 3 units again based on total time. Your bill would need to have 2 units of therapeutic exercises which equals 30 minutes with 2 minutes remainder. You don’t meet the 8 minute requirement for manual therapy alone because of the 7 minutes but since it is more than the 2 minutes remaining from the therapeutic exercises you add those minutes to the 7 minutes and can now bill for 1 unit of manual therapy.
One more example:
7 minutes of manual therapy + 8 minutes therapeutic activities + 7 minutes of patient education Self-care/Home Management Training = 21 minutes
Because the total time is only within the range for 1 unit that’s all you may bill. The procedure with the most minutes is therapeutic activities to you would bill 1 unit of that code and include the other minutes in that billing.
The 8-minute rule is generally only applicable to Medicare patients. Other third party payers typically use the midpoint rule where you may bill one unit for any timed procedure or modality that you perform for 8 or more minutes. The total time requirement is not in play here. As always, this does depend on your payer contracts so be sure you know those details as well as any updates in these rules for these payers.
How do you bill if you total enough minutes for 3 units but don’t have at least 8 minutes left after billing the full 15 min units?
Suppose you provided 30 minutes of Therapeutic Exercises, 6 minutes of manual therapy and 4 minutes of Therapeutic Activities which totals 40 minutes. In this case you may bill 3 units total. You would bill 2 units of Therapeutic Exercise, but you don’t have 8 minutes of either Manual Therapy or Therapeutic Activities. CMS directs you to add these two together (equaling 10 minutes) and you may bill whichever code has more minutes provided. Your 3rd unit would be billed as Manual Therapy because you provided more (6 minutes) than Therapeutic Activities (4 minutes).
Let’s say your treatment was 25 minutes of therapeutic exercises, 20 minutes of cervical mechanical traction and 13 minutes of therapeutic activities. You total the Therapeutic Exercise minutes and the Therapeutic Activities minutes which equals 38 minutes. You would bill 2 units of Therapeutic Exercises and 1 unit of Therapeutic Activities for the timed codes. However, since the Cervical Mechanical Traction is an un-timed code you bill 1 unit.
CMS allows you to include any time spent re-assessing the patient or teaching the patient about how to manage their problem. For example, if you are re-assessing a patient’s balance or coordination after having done some Neuromuscular Re-education techniques then you may include that time in the minutes spent doing the Neuromuscular Re-ed. By the way the clock starts running as soon as you interact with the patient. So, if you get your patient from the waiting room and ask how they are doing (e.g. seeking their current status) and observe their gait or their movments then you have started your assessment. Likewise if you are teaching the patient some new exercises for their home program or if you were teaching them safer movement patterns when getting out of bed you would be able to include those minutes in the Therapeutic Exercise time or the Therapeutic Activities unit time.
Not exactly. Like CMS they do still require you to provide more than half of the 15 minutes of any unit to bill for that unit. Most do not use the total time to determine the total number of billable units. Thus, if you provided 8 minutes of Manual Therapy, 10 minutes of Therapeutic Exercises and 8 minutes of Neuromuscular Re-education totaling 26 minutes, under Medicare you could only bill 2 units. For most commercial health insurers, you could bill 1 unit for each of those codes which is 3 units total.
If you are doing any documentation in front of the patient (for that patient) during your intervention work with them, you may include that in your minutes. However, you may not include any documentation time done away from the patient. CMS generally states that time spent writing notes away from the patient is non-billable.
Yes, but only if you do additional interventions on that date of service. The Initial eval code is an untimed code. No matter how long or complex it is there is no time definition for the initial eval. If you do additional interventions that day, such as initiate some manual therapy or therapeutic exercises, you would total the minutes spent on those timed codes and bill the appropriate units as described above.
First, your documentation must clearly support the level of intensity and direct one-on-one time spent on any timed codes being billed. It must also clearly match with the definitions in the CPT code book for that code. The default as to which code a specific intervention is allocated to is based on intent. For example, if you are doing sit to stand exercises for the purposes of strengthening the lower extremities then that would be counted in the Therapeutic Exercise time. If you are doing that exercise to help a patient improve their ability to rise from a chair then it could be counted under the Therapeutic Activities time.
The 8 minute rule is nothing to be afraid of. With a clear understanding of what the rule means you can ensure that you’re not over billing or under billing. You deserve to be paid for the services you provide in accordance with Medicare’s rule. MWTherapy can help you with Medicare compliance giving you built-in tools to help keep you on track.